Purulent drainage—also known as purulent exudate or pus or Purulent discharge—is a thick, often milky discharge that comes from an infected wound. It’s rich in dead white blood cells, bacteria, and tissue debris, indicating that your body’s immune system is actively fighting an infection.
Purulent Drainage Color & What It Looks Like
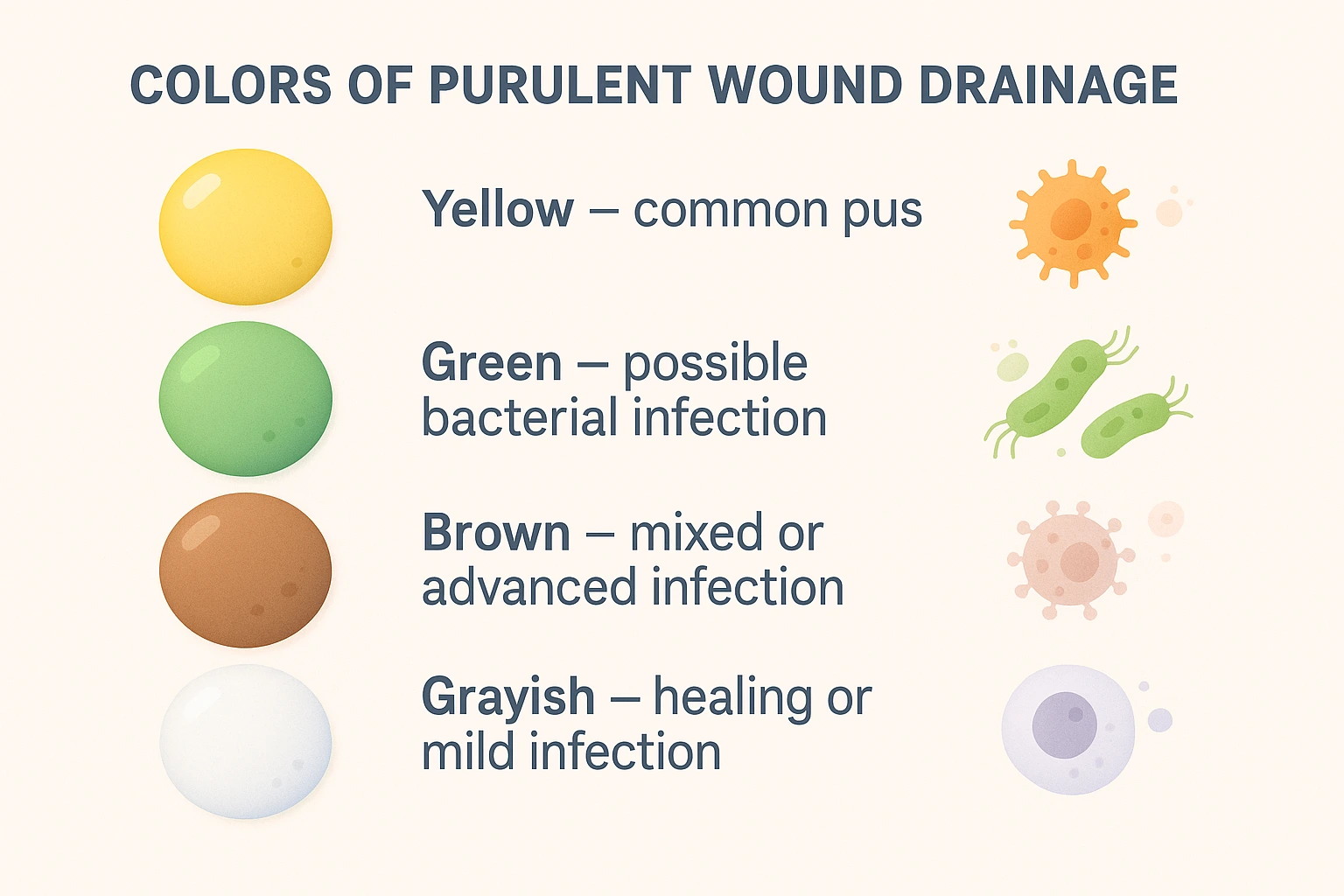
Purulent wound drainage can vary widely in color—from grayish or yellow to green or brown—and often appears thick, opaque, or milky. Yellow pus from the wound or thick yellow or green discharge are classic signs. The change in color typically reflects the presence of cells like neutrophils and dead bacteria.
The appearance of white‑blood‑cell‑rich pus results from immune activity, while a foul‑smelling wound discharge may suggest a particularly aggressive or advanced infection.
Wound Drainage Types: Serous vs Purulent
Knowing how to differentiate drainage types is essential for assessing healing:
- Serous Drainage is clear, watery, and typical in early wound healing. It’s usually translucent and light.
- Serosanguineous Drainage is a mix of serous fluid with a small amount of blood—slightly pinkish—but generally normal for recovering wounds.
- Sanguineous (fresh blood) or hemorrhagic drainage indicates abnormal bleeding and may require urgent attention.
- Purulent Drainage, as described, is thick, colored, and often smelly, which is abnormal and indicative of infection.
Signs of Infection & When to Seek Help
Signs of purulent drainage or discharge and infection include:
- Thick, milky, yellow/green/brown discharge (pus in the wound)
- Strong, unpleasant odor
- Increasing amount of drainage
- Redness, swelling, warmth around the wound
- Fever, increasing pain
- Development of an abscess—a painful, fluid‑filled lump beneath the skin.
Is purulent drainage normal? No—it’s a red flag. If you see it—or notice a foul-smelling wound discharge—contact your healthcare provider promptly.
Causes of Purulent Drainage
Purulent exudate forms because the body sends white blood cells to fight infection. When these immune cells—and the invading pathogens—die off, they accumulate to form pus. Abscesses, common causes of purulent drainage, are pockets of pus that need drainage.
How to Treat Purulent Discharge?

Medical Treatment Options
- Assessment & Culture
To tailor treatment, clinicians often perform a wound culture using methods like the Levine technique to determine the infecting microbe. - Antibiotics
Early intervention usually involves oral or topical antibiotics, depending on severity and culture results. - Incision and Drainage (I&D)
If an abscess is present, a minor surgical procedure may be used to release pus effectively. For many uncomplicated abscesses, I&D alone (without antibiotics) may suffice. - Advanced Wound Dressings
Moisture-balancing dressings, such as alginate wound dressings, help absorb excess exudate and support healing; they often need changing every 2 days. Other advanced treatment options may include negative pressure wound therapy. - Hyperbaric Oxygen Therapy (HBOT)
Hyperbaric Oxygen Therapy (HBOT) can enhance healing for certain infected or chronic wounds by delivering high-pressure oxygen, improving blood flow, and supporting immune cell function. - Emerging Therapies
In some cases, treatments like growth factors, bioengineered tissues, bacteriophage therapy, and stem cell applications may accelerate healing.
At-Home Care (With Medical Guidance)
Between medical visits, proper wound care is vital:
- Gently clean around the wound with mild soap or saline
- Remove debris carefully with clean tools
- Apply antiseptic and use clean, appropriate dressings
- Follow provider’s instructions and avoid aggressive scrubbing.
Understanding Wound Healing Stages, Inflammation & Pus
The healing stages of wound are:
- Hemostasis – Blood clotting
- Inflammation – Immune cells arrive, sometimes producing pus
- Proliferation – New tissue forms
- Remodeling – Strengthening until healed
Purulent drainage often emerges during prolonged inflammation, indicating the body is still fighting infection rather than moving forward in healing.
When to See a Doctor
Contact a healthcare provider immediately if you notice:
- Thick, colored (yellow/green) or foul‑smelling drainage
- Worsening redness, swelling, or pain
- Fever or feeling unwell
- A tender lump that’s warm—suggesting an abscess
- No improvement after a few days of proper care
Ignoring purulent drainage can lead to chronic wounds, deeper infections, or sepsis—risks that are best avoided through timely intervention.
Final Thoughts
Dealing with purulent wound drainage can be alarming, but understanding what it is, recognizing the signs, and knowing when and how to act empowers patients in their wound-healing journey. With the proper combination of professional care—such as antibiotics, wound cultures, I&D, advanced dressings, or even HBOT—and at-home support, healing can resume on track, turning inflammation and infection into recovery and renewed health.
If you’re exploring advanced treatments like hyperbaric oxygen therapy for infected wounds, you’re already taking proactive steps toward optimal care. Always partner with your healthcare team to tailor the best path forward.
FAQs
1. Is yellow pus always a sign of infection?
Not always. While yellow or green pus often suggests infection, sometimes drainage may occur as part of the body’s normal healing response. If pus is persistent, increases in amount, or is accompanied by pain, swelling, or fever, it’s best to see a healthcare provider.
2. Can purulent drainage heal on its own?
Mild purulent drainage may sometimes improve with proper wound care, such as cleaning and covering the area. However, if purulent discharge continues, worsens, or is associated with other symptoms like redness, warmth, or fever, medical treatment may be necessary to prevent complications.
3. How long does purulent drainage last?
The duration depends on the cause and the body’s healing process. Minor cases may resolve in a few days with good hygiene and care. But if purulent drainage lasts longer than a week, does not improve, or becomes more severe, it usually indicates infection and requires medical evaluation.
4. What if purulent drainage has blood in it?
A small amount of blood mixed with drainage can happen if the wound is irritated or the tissue is healing. However, heavy bleeding or persistent blood-streaked pus may signal a more serious infection or tissue damage. It’s important to have this checked by a healthcare provider.
5. Does foul-smelling drainage always mean infection?
Foul odor often suggests infection, especially when combined with thick pus, swelling, or redness. However, not all bad-smelling discharge is caused by bacteria—sometimes dead tissue or other factors can cause odor. To be safe, any foul-smelling purulent discharge should be evaluated by a medical professional.